The final 2 weeks of the CSC visit to the UK included time spent at Southmead Hospital, University of the West of England, and a visit to the House of Lords hosted by Lord Nigel Crisp:
This report synthesizes key insights into Bristol’s stroke care ecosystem, emphasizing leadership models, clinical innovations research frameworks, and partnership opportunities for transferable strategies to enhance stroke outcomes in Northern Ghana and The Gambia.
Leadership and Service Integration:
Bristol’s stroke units exemplify adaptive leadership and operational efficiency. They support dynamic staff empowerment with nurses trained in NIHSS scoring and therapists empowered to screen for thrombolysis. Daily ‘safety huddles’ enable real-time incident reporting and resource allocation. A ‘dynamic zoning’ model alongside enhanced staff flexibility for their 43 stroke beds eliminates mid-pathway transfers between acute and rehab settings.
Clinical Skills and Knowledge Transfer:
Bristol’s ‘low-tech, high-skill’ philosophy aligns with West African resource reality. Standardized dysphagia screening (bedside water tests/video-fluoroscopy), reduced pneumonia rates by 18%. Early mobilization (<24 hrs post-stroke) using cost-effective tools like bamboo parallel bars promotes positive outcomes. Specialized clinics cohorting groups of patients such as young stroke or TIA enables streamlining of diagnostics and increased awareness of less common aetiologies such as sickle cell disease.
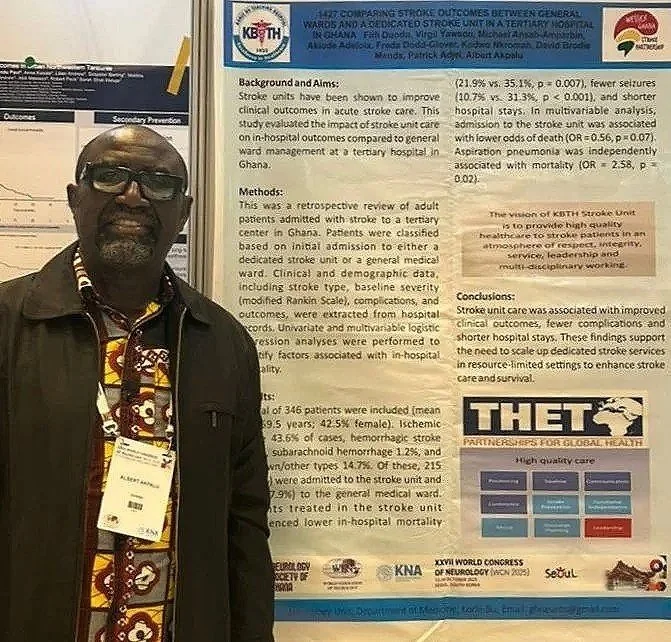
Research and Data-Driven Care:
Bournemouth and Bristol’s research infrastructure both offer templates for evidence-based care in Ghana and The Gambia. The UK Sentinel Stroke National Audt Programme (SSNAP) tracks outcomes (e.g. door-to-needle time), enabling quality improvement. Both Ghana and The Gambia could benefit from a nationalized data approach to stroke care.
Bristol participates in research showing telehealth efficacy which could be transformational in low resource settings such as Ghana, where 54% of healthcare professionals report knowledge gaps in post-stroke rehab . Dr. Akwulpwa advocates integrating WGSP’s 8 core skills online modules (e.g. swallowing, positioning, continence management) into staff and family training programmes.
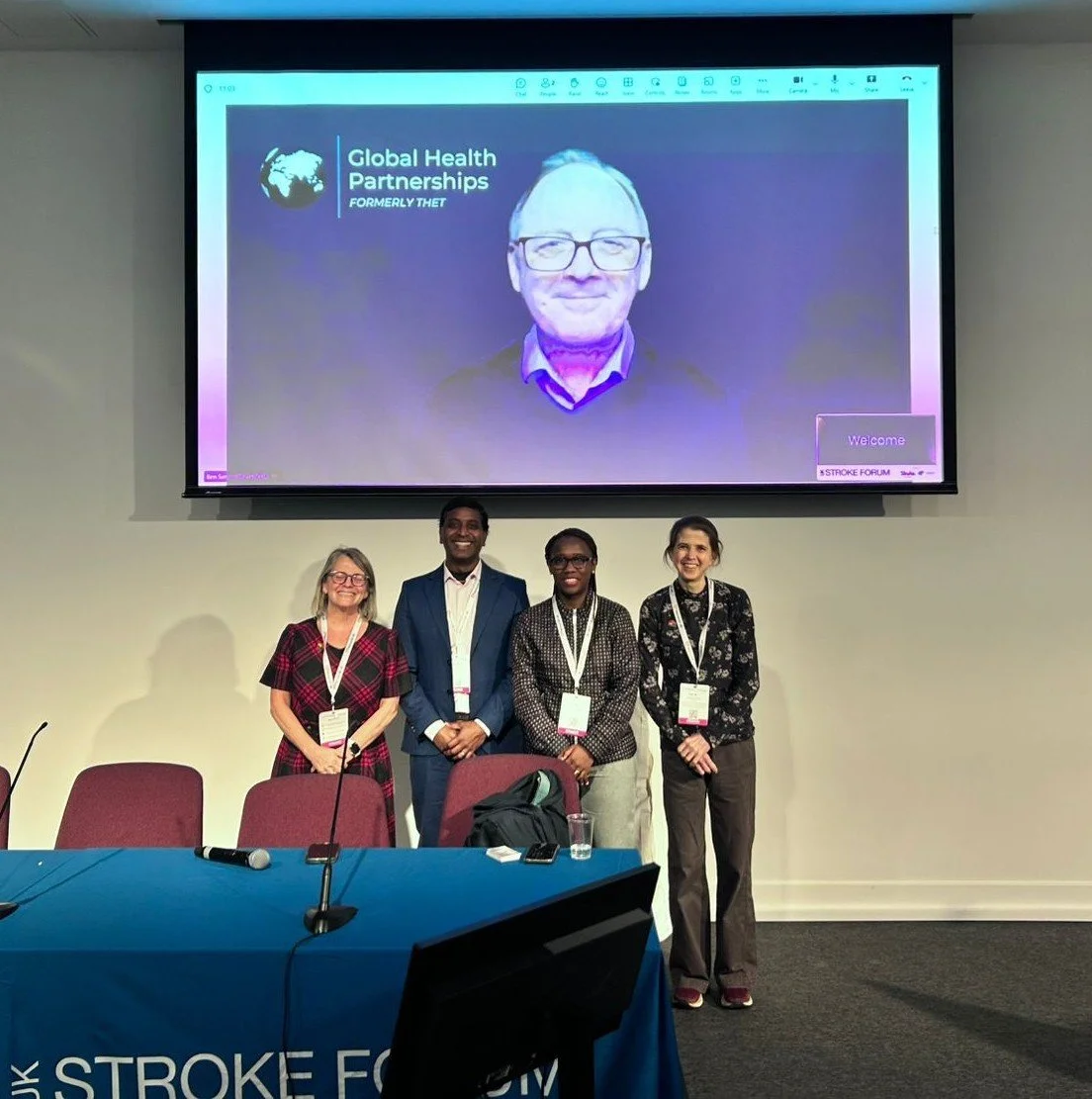
Partnership and Collaborative Frameworks:
Opportunities for skills sharing across WGSP partners includes NIHSS stroke assessment training, protocol design/development based on current in-country templates, and telemedical support for decision-making.
Challenges:
Resource limitations: Tamale Teaching Hospital, Ghana’s non-functional MRI scanners delay diagnostics. Variable availability of CT imaging in The Gambia due to cost to patient and scanner reliability restricts treatment options for patients.
Workforce gaps: Neurologist density remains critically low with only 1:4 million population in Northern Ghana. There are no native neurologists in the Gambia (population 2.5 million).
Recommendations:
1. Leadership development: workshops on "crisis leadership" and advocacy to navigate administrative challenges.
2. Frugal innovation: co-develop low cost tools, such as the realistic dysphagia screens in use by WGSP partners, shared via WGSP networks.
3. Tele-mentorship: virtual case discussions between WGSP partners.
4. Joint funding proposals: target grants (e.g. CSC, Global Health Partnerships) for staff training.
“The partnership exemplifies sustainable change through equity.” Dr Valentine Akwulpwa.